Vertical Dimension of Occlusion (VDO) in Clinical Practice: What I’ve Learned From Years in the Trenches
I’ll never forget my first prosthodontics class in dental school. My teacher held up two plaster models—one had a flat, collapsed bite, the other looked tall and healthy. “The Vertical Dimension of Occlusion,” she said, “decides everything from how your patient eats to how they look in the mirror.” I was hooked. Since then, I’ve spent years checking, fixing, and adjusting VDO in all kinds of situations, from rehabbing a whole mouth to tricky denture problems. Here’s what I’ve learned.
Table of Contents
What Is Vertical Dimension of Occlusion (VDO)?
Vertical Dimension of Occlusion (VDO) is just a fancy way to say the height between your top and bottom jaws when your teeth are biting together. Imagine clapping your teeth together—where your jaws stop moving, that’s your VDO. It sounds simple, but things get tricky fast.
In my experience, there isn’t one “correct” VDO for everyone. Getting it right makes the difference between comfort and pain, working teeth and broken ones, and a smile you want to show off or hide. Since everyone’s jaws, teeth, and muscles are different, I’ve learned each person has their own perfect VDO—not just whatever the book says.
VDO vs VDR and Freeway Space: Clearing Up Confusion
Early on, I used to mix up VDO with two other important words: Vertical Dimension at Rest (VDR) and Freeway Space. Here’s how I explain it to my patients (and sometimes to myself when I need a reminder):
- VDR is the space between the jaws when you’re relaxed, lips together, teeth apart.
- VDO is the space when your teeth are shut together, biting in your normal way.
The gap between VDR and VDO is called the Freeway Space (or interocclusal rest space). Most books and studies say this space should be 2-4 mm in the premolar area. If it’s bigger or smaller, something might be off with the patient’s VDO.
I think of freeway space like the gap in your car brakes when you’re not pressing the pedal. Too little, and something’s always tight; too much, and nothing works right.
Why VDO Matters: Beyond Just Teeth
When I started out, I thought VDO only had to do with the teeth. But it’s much more:
- How you look: Get it wrong and you see deep wrinkles, sagging cheeks, and a flat face that can wreck someone’s confidence.
- Jaw Joints: The TMJ needs the teeth and muscles to work together just right. Mess with the VDO, and your jaw joint will let you know.
- Speaking: A VDO that’s too high or too low can make it hard to say certain words. Try saying “fifty-one” or sipping soup with the wrong bite—you’ll see.
- Eating and Swallowing: A bad VDO can make chewing tough, swallowing weird, and your jaw muscles tired or sore.
So, in my work, even small changes in VDO feel big—they touch everything from bones to speech and self-image.
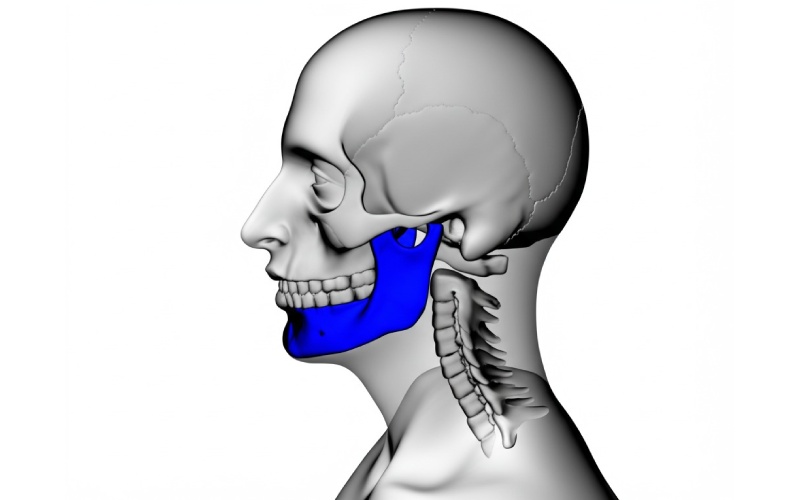
The Anatomy Behind VDO: Muscles, Joints, and Bones
If you want to get VDO right, you have to know the basics. Here’s the quick guide I wish I’d had:
- TMJ (Jaw Joint): This is like a hinge and slider in one. Changing the VDO shifts the jaw joint, sometimes causing pain or clicking.
- Chewing Muscles: The masseter, temporalis, and pterygoids all have their own ideas about jaw position. Sometimes even tiny bite changes make the muscles sore or tired.
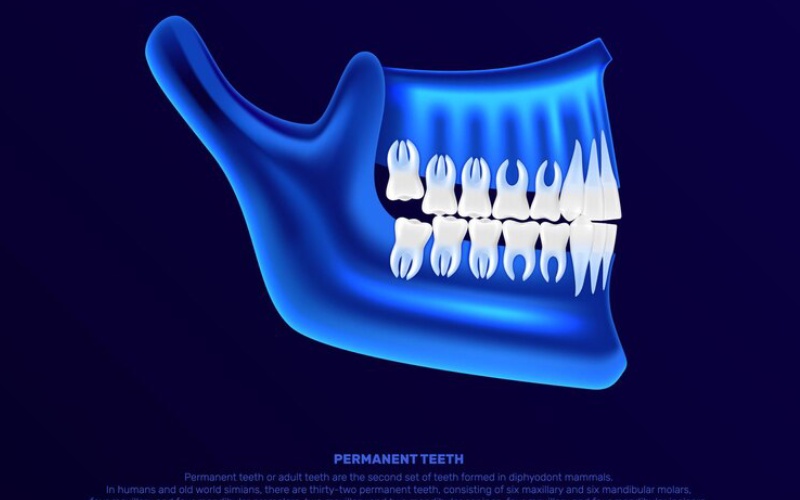
- Jaw Bones and Teeth: Over time, losing teeth or jaw bone brings your jaws closer, dropping the VDO and making people look older.
Knowing this has saved me a lot of trouble in planning treatment and fixing problems.
How I Check VDO in Patients
When someone comes in with worn teeth, loose dentures, or jaw pain, I start my exam broad and then zoom in.
Full Patient Checkup
First, I listen. People often describe problems—new face wrinkles, tired jaws, speech troubles, or denture gripes—that hint at VDO problems. I look for lost face height, cracked mouth corners, and sore jaw muscles.
Ways I Test VDO
I’ve tried lots of tricks over the years. Each has its ups and downs, so I mix a few together:
1. Phonetic (Speech) Test
I ask folks to say words with “S” or “F/V”—like “fifty-five” or “seven.” These sounds pull the top and bottom teeth close but not touching. Weird speech hints the VDO is off. It’s fast, simple, and surprisingly useful.
2. Face Measurements
The old Willis Gauge is still handy. I measure from below the nose to the chin—first with lips just resting, then with teeth together. Comparing the numbers helps me spot lost VDO. Sometimes, I’ll use the Niswonger Method for backup.
3. Feel Test
Wax rims and trial teeth let me “try out” a new VDO in the patient’s mouth. I watch for better lip support, fuller cheeks, and how comfy it feels. Letting patients test the new height is like trying on a suit before you buy it—huge help for both me and the patient.
4. Muscle “Reset”
Sometimes tight muscles mess up your measurements. Tools like the Lucia Jig or Leaf Gauge let the muscles relax so I get a true jaw position.
5. Digital Tools
Now, digital stuff—like mouth scanners, CBCT, and computer models—are part of my everyday work. Research shows they are as good as, or even better than, old-school ways—sometimes picking up changes as tiny as 0.5 mm.
6. X-Ray Analysis
For tricky jaw and tooth relationships—like braces or jaw surgery—I use head x-rays (cephalometrics). It’s more “still picture” than live action, but gives good facts.
Clear Signs: Is the VDO Wrong?
I’ve seen a few dead giveaways that VDO isn’t right:
- Too Low (Collapsed): Look for a flat lower face, lips closing too much, deep lines from nose to mouth (“marionette lines”), tired muscles, or cheek and tongue bites. Chewing gets harder, and people look older.
- Too High: Trouble closing lips, strange-sounding speech (“th” with a whistle), gagging on dentures or new teeth, sore muscles, and headaches.
Most of the time, patients just know something feels “off”—not what it is. My job’s to spot these clues and find the VDO problem.

What Happens When You Mess With VDO (Too Low or High)
VDO Falls Too Low
I once saw a 55-year-old guy with bad jaw pain, chewing problems, and a lower face that looked melted. Teeth grinding and years of wear dropped his VDO. Stats back me up: about 70% of folks with low VDO have jaw pain or clicking.
The good news? Raising the VDO, carefully and slowly, often fixes it—like it did for him with a mouthful of new crowns. After we finished, he had zero pain and looked years younger.
VDO Goes Too High
On the flip side, I raised a patient’s VDO too much once (a rookie mistake). A few days later, she came back: sore jaw, tight lips, strange speech, could never find her bite. Studies say if you push the VDO more than 3-5 mm too fast, it usually backfires.
But, if you lift it slowly, watch closely, and use trial teeth, most people can adapt. Sprinting through the steps means failures and unhappy patients.
How I Restore VDO (and Keep it Good)
My Step-by-Step Way
- Look and Plan First: Don’t fix VDO unless you check everything—face, speech, muscles, x-rays, and all.
- Try With Temporary Teeth: Before you do crowns or dentures for good, use “test run” teeth so the patient, and their jaw, can adjust. Less drama this way.
- Work Together: My best results came teaming up with orthodontists, surgeons, or physical therapists.
- How I Actually Build Teeth:
- For whole mouth makeovers, I mix crowns, onlays, or veneers. The stuff I pick matters for how long it lasts.
- Dentures are big for older folks or those with lots of wear—and implants can help steady things while you adjust VDO.
- Implants made huge improvements for keeping VDO stable and predictable.
- Try an Occlusal Splint: If I’m unsure, I make a splint (mouth guard) at the new VDO first, to test how the jaw and muscles handle it.
Important Research Points
The evidence is strong: full mouth VDO changes work 85-95% of the time over 5-10 years—if you respect the steps. Most trouble comes from skipping basics.
What Happens Over Time: What Works, What Fails
I’ve followed lots of my VDO cases for years. The happiest had a few things in common:
- I raised their VDO slowly, not all at once.
- I checked on them often during the “getting used to it” phase (usually 2-6 weeks of temps).
- I made sure they knew what to expect and fixed small things fast.
- Regular checkups kept little issues from blowing up.
Bottom line? Being careful, taking your time, and working together is the secret.
Real Patient Story and What the Latest Research Says
Let me give you a quick story:
Case: Collapsed VDO and Full Mouth Rebuild
A patient with really worn down teeth and sore muscles came in, looking exhausted. I checked over everything: the freeway space, speech, how the muscles felt. It looked like raising the VDO by 4mm would help. We tested it with temporary crowns for a month. Tiny tweaks got rid of discomfort. Three years later—with permanent crowns—he still felt great and looked younger.
Newest research matches my results. Restoring lost VDO helps 75-85% of jaw pain cases. Digital methods like computer scanning now let me get within 0.5-1 mm of perfect—less guessing, more happy smiles.
My Best Advice: Key Rules of Everyday Work
Here’s what all my years have taught me:
- There’s no one-size-fits-all VDO—every patient is different
- Mix what the patient says (comfort, looks, speech) with what you measure (numbers, scans)
- Start with temp teeth—let the jaws get used to it before you make it final
- If in doubt, go slower and make small changes. It lasts longer that way
- Don’t try to be a hero—bring in teammates for the tough cases
- Write it all down and teach your patients as you go
What’s Next for VDO?
The digital world is changing everything. Virtual “jaw testers”, 3D scanning, and computer-made teeth aren’t just for fancy labs now. These gadgets make VDO checks more repeatable, less “guess and hope,” and let the patient see what’s going on.
I’m also seeing way more teamwork—prosthodontists, orthodontists, jaw surgeons, and therapists all pitching in, especially for patients who care both about looks and how their jaws work.
Final Thoughts: Why Mastering VDO Changed My Practice
Years ago, I thought VDO was just another number, another box to tick. Now, I see it’s the foundation beneath everything I do in prosthodontics. When I get the VDO right, my patients look better, chew easier, and feel more like themselves. Careful checks, smart planning, and real follow-ups turned VDO cases from a headache into some of the most rewarding in my whole career.
If you’re facing a tough case or just want to get better at this, remember: VDO isn’t a riddle once you learn the parts and stay patient. And once you really nail it, your whole view on dentistry changes for the better.
Further Reading & References
- Dawson PE. Functional Occlusion: From TMJ to Smile Design.
- Boucher CO. Prosthodontic Treatment for Edentulous Patients.
- Clinical trials and reviews mentioned above.
If you’ve got cases or questions about VDO, reach out or drop a comment. I’m always happy to share more tips or help you sort things out. Happy treating!