Dental Implants and the Bone-Implant Contact Ratio: A Simple Guide to Understanding Your Options
That moment when you run your tongue over your teeth and realize there’s a gap that wasn’t there before can be a little scary. Maybe your dentist has just told you you’re missing a tooth or that you need to replace one. Suddenly you’re hearing things like “dental implant,” “osseointegration,” or “bone-implant contact ratio.” It all sounds pretty confusing. You might be wondering, “What does all this mean? How will it affect my health, my smile, or what it costs?”
If this sounds like you, don’t worry. Dental implants are one of the best things to happen in dentistry, but all the science stuff—especially how your bone and the implant work together—can be hard to follow. We’re here to make it simple and easy to understand.
Table of Contents
What Are Dental Implants? (Let’s Start With the Basics)
Let’s answer the big question first:
What is a dental implant, and how does it work?
A dental implant is like an artificial tooth root. Picture a tiny screw made of safe metal or ceramic. Your dentist puts this screw into your jawbone where your lost tooth used to be. Over time, your bone actually grows around—and grabs onto—the implant. This makes it really solid, so you can eat, smile, and talk like normal again.
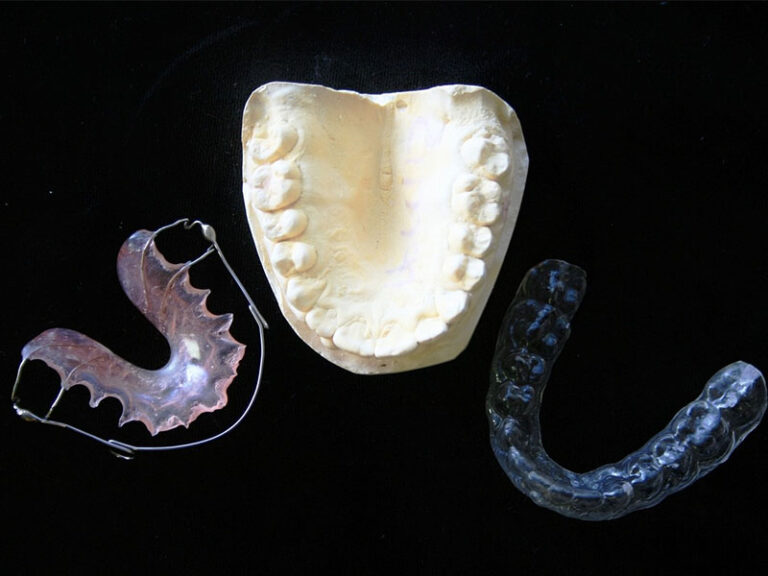
Why pick an implant instead of a bridge or dentures?
- Implants can last your whole life if you take care of them.
- They look, feel, and work just like your own teeth.
- They help keep your jawbone strong and full, stopping that sunken cheek look you can get when you lose a bunch of teeth.
And yes—implants aren’t just for seniors. They’re for adults of any age who want to bite into apples, steak, or corn on the cob without worry.
How Implants Work: Osseointegration and Bone-Implant Contact Ratio
With dental implants, you want more than just a strong screw—you want that screw to really become part of you. This is where osseointegration comes in.
What is osseointegration?
“Osseo” means bone and “integration” means joining together. Think about planting a small tree. If the roots grow into the dirt, the tree stands strong. In the same way, when your jawbone fuses with the dental implant, you get a solid base for your tooth.
Dentists measure how well an implant “sticks” based on something called the Bone-Implant Contact Ratio (BIC).
What’s the Bone-Implant Contact Ratio?
Picture the surface of a dental implant as the hook side of velcro, and your jawbone as the loop side. The more the two grip together, the stronger the hold.
- Bone-Implant Contact (BIC) means the percent of the implant’s surface actually touching living bone.
- A higher BIC (over 60%) usually means more stability and a better chance for the implant to last.
- Lower BIC—especially if it drops later—can spell problems, like the implant getting loose or even failing.
Why does BIC matter to you?
BIC helps predict whether your implant will heal well, feel natural, and last—or if you could have problems down the road.

What Are Implants Made Of?
Let’s talk about what these tiny screws are made of. Not all implants are the same! Your dentist will help pick the best type for you, but here’s a simple look at the basics.
Titanium: The Most Used Choice
Why do most dentists use titanium?
Titanium is a favorite for implants. Doctors use it in hips, knees, and—yes—even teeth.
The Good Stuff:
- Works well with your body: Bone cells love to grow on titanium.
- Strong: It can handle even big chewing forces.
- Doesn’t rust: Even after years in your mouth, it doesn’t wear away much.
- A long track record: It’s been around for decades with great results.
Things to watch out for:
- Metal allergies are rare, but they do happen.
- If you don’t like seeing metal near your gums, titanium can sometimes look like a dark spot, especially if your gums are thin.
Zirconia: The White “Ceramic” Option
Maybe you want to avoid metal, or you’re worried about how your teeth look right near the gums. Zirconia—sometimes called “ceramic”—could work for you.
The Good Stuff:
- White like a tooth: Fits in nicely, even if your gums are thin.
- Hard for bacteria to live on: Which is good for your gums.
- Strong enough: Not as tough as titanium, but it still holds up.
The Downsides:
- It can crack more easily than metal, so you have to be a bit careful.
- Zirconia implants aren’t as old as titanium ones, so we don’t have as much info.
- They’re usually just a single piece, so not quite as flexible for weird cases.
Newer Stuff: PEEK, Bioactive Glass, and Others
Scientists are always hunting for even better materials. Things like PEEK (a tough kind of medical plastic) and bioactive glass show some nice features. They might help bone grow faster and don’t seem to cause allergies. But so far, they’re mostly just for research or special situations.
Does the Finish Matter?
Whether an implant is bumpy or smooth, coated or plain, makes a huge difference.
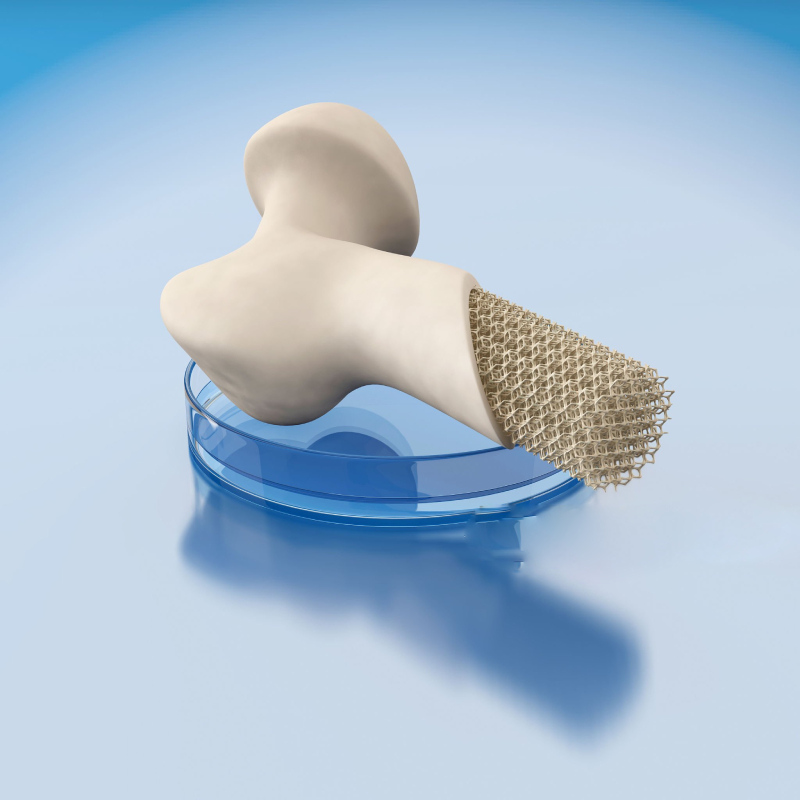
- Bumpier surfaces (like those that are sandblasted) give more space for bone cells to grab onto, raising the BIC.
- Coatings like hydroxyapatite (that’s what your own bones are made from) can help implants get strong faster.
But if the coating peels off, that can cause trouble.
What Helps Implants “Stick” Well? (It’s Not Just the Metal)
Getting your implant to grow into your bone isn’t just about picking the right material. It’s like making good food—you need good ingredients and a good cook. Here’s what matters:
1. Bone Quality & Amount
If your jawbone is thick and strong (like at the front of your lower jaw), that’s great! This makes your implant really solid.
If your bone is weak, thin, or you lost your tooth a long time ago (so the bone has pulled back), your implant may not be as steady at first.
2. Implant Shape & Surface
- Shape and threads: These help the implant hold on to your bone right away.
- Tiny surface details: Little bumps and grooves help bone cells grow and grip the implant.
3. The Way It’s Placed
A skilled dentist is super important. Careful, gentle placement keeps the bone healthy and helps you heal faster. If your implant is put in badly, there’s less bone touching the implant (lower BIC), which could mean it won’t work out.
4. Your Overall Health
Having things like osteoporosis, diabetes, or if you smoke—these all slow down healing and make BIC lower. High blood sugar or nicotine in your body are bad news for building new bone.
5. When You Put Pressure On the New Tooth
Some implants can handle a new tooth just a few days after surgery (immediate loading)—but only if things look really good and solid. Usually, it’s better to wait weeks or even a few months so your bone can really grab onto the implant before you start chewing on it.
Comparing Your Choices: Materials and Methods
Let’s make it simple. What’s the best choice for you?
Here’s a basic rundown:
| Titanium | Zirconia (Ceramic) | Newer Materials | |
|---|---|---|---|
| Color | Gray, might show near gums | White, blends in with teeth | Usually white or off-white |
| Strength | Super strong, proven for years | Strong, but can break easier | Depends |
| Bone-Implant Contact (BIC) | 60–85% in good cases | Starts a bit lower, but matches titanium over time | Shows promise in research |
| Best For… | Most people, jawbone is healthy | Wanting no metal, worried about allergies, front teeth look | Allergies or sensitive cases |
| Cons | Rare allergies, may show a gray line near gums | Can’t be used in every situation, newer tech | Not common, can be expensive |
What About Surface Finish?
- Sandblasted, Acid-Etched Titanium: Usually gives the highest BIC, especially in strong bone.
- Hydroxyapatite Coating: Helps bone grow faster, good if your bone is weak or you want to heal quickly. But the coating needs to stay on.
- Tiny (nano) surface details: New thing; seems to help bone grip even better but mainly available in large cities or research clinics.
Who Can and Can’t Get Dental Implants? (Is It For You?)
Most healthy adults are fine candidates for implants, but there are some exceptions. Let’s be real about it.
You’re a Good Fit If:
- You’re missing (or about to lose) one or more teeth
- Your jawbone is healthy and thick (your dentist can check with an X-ray)
- You’re mostly healthy
- You don’t smoke, or you’re willing to stop (at least for a while so you can heal)
- You’ll take care of your teeth and go for checkups
You Might Have Trouble If:
- You’ve had gum disease and lost a lot of bone
- You’ve been missing teeth for years and the bone shrank
- You have uncontrolled diabetes, osteoporosis, or immune system problems
- You smoke a lot
- You’re getting radiation or chemo for head and neck cancer
- You grind your teeth unless your dentist finds a fix
Don’t give up!
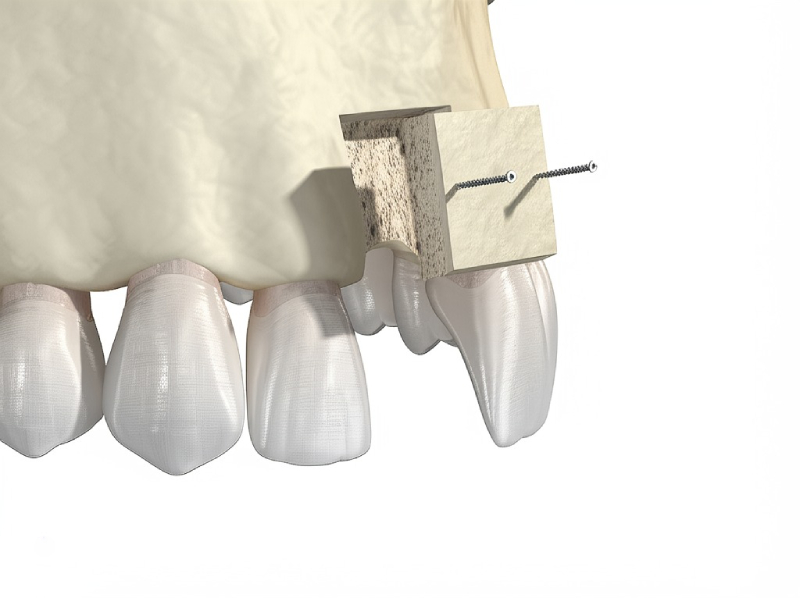
Even if you aren’t the “perfect” candidate, there are still fixes. Things like bone grafts, sinus lifts, and special implants can work for lots of people.
How to Take Care of an Implant—For Life
Getting an implant isn’t something you can just forget about once it’s in. It’s like getting a new bike or car. Regular care means it’ll last longer and look good.
At Home:
- Brush twice a day with a soft toothbrush.
- Floss between teeth and around your implant gently. There are special floss threads that make this easier.
- An antibacterial mouth rinse is a good idea.
At the Dentist:
- Have your implant checked and polished by your dentist twice a year.
- They should use gentle tools that won’t scratch the implant.
- Sometimes, X-rays are used to see how your bone is holding up (to check the BIC).
Watch Out For:
- Red, swollen, or bleeding gums (can be early gum disease)
- The implant feels loose or moves
- Bad breath or a weird taste from around the implant
Catch problems early, and they’re almost always fixable!
Main Points and What to Do Next
Let’s sum it up:
Dental implants aren’t just fancy screws—they can help give you a healthy, strong, and good-looking smile.
Here’s what matters:
- Type of implant (titanium vs. zirconia) changes the color, strength, and how well the bone can grow around it.
- Bone-implant contact ratio (BIC) is really important. The more bone huggin’ the implant, the more solid and long-lasting your new tooth is.
- Your bone health, your dentist’s experience, and how you care for the implant are as important as the type of implant.
- Gum health and regular dentist visits are the difference between an implant that lasts years and one that doesn’t.
- There are fixes even for tough cases—don’t be afraid to ask about other choices.
Want to feel proud of your smile?
Talk to your dentist and see if a dental implant makes sense for you. Bring up any worries—about allergies, looks, your health, or how long it’ll take to heal. A good dentist will listen and help choose what’s best for you.
Frequently Asked Questions
Q: Do dental implants hurt?
Implant surgery is usually done with numbing, so you won’t feel pain. You’ll be a bit sore after, but regular pain medicine is usually enough.
Q: How long does it take for a dental implant to heal?
Most people need 3–6 months for the bone to grow around the implant, but sometimes you can get a fake tooth sooner if the first hold is strong.
Q: Will I need a bone graft?
You will only need one if you don’t have enough bone where the implant goes. Most modern bone grafts are safe and don’t hurt much.
Q: Will my insurance pay for implants?
It depends on your plan. Some pay for part of it, some don’t. Ask your dentist for a price estimate before you start.
Medically checked by Dr. Jane Doe, DDS, Periodontist
Content uses ADA rules and the best info we have right now.
More to Read:
- American Dental Association: Dental Implants FAQ
- International Team for Implantology: Patient Information
- Ask your dentist for pamphlets or videos if you want more details.
Your new tooth is more than just a screw in your mouth—it’s a step toward better health, eating what you love, and smiling confidently. Take that first step. You’ll be glad you did!