A Physician’s Guide to Dental Solutions for Sleep Apnea
That Annoying Snore Isn’t Always So Innocent: Is There a Dental Solution for Sleep Apnea?
If you—or someone you care about—wakes up gasping for air, feels tired all day, or has heard, “You’ve got sleep apnea,” it’s normal to be a bit confused. Maybe you even tried the CPAP machine and found it uncomfortable, loud, or just tough to use. Or maybe you’ve wondered if those mouth devices dentists talk about actually help.
Let’s be clear: you’re definitely not alone, and your questions make sense. Obstructive sleep apnea (OSA) is common and can be risky, but new ways in dental care can help more than ever before. Curious about those dental gadgets for sleep apnea? Want to know if they really work, are safe, and doctors actually use them? You’re in the right spot. Let’s clear things up, using facts—not fluff—so you can sleep better starting tonight.
Table of Contents
What is Dental Appliance Therapy for Sleep Apnea?
Understanding Oral Appliance Therapy (OAT)
Think of your airway at night like a garden hose. When you sleep, the muscles in your throat relax. For some people, their tongue or jaw drops back and squeezes the “hose,” making breathing hard. Obstructive sleep apnea (OSA) happens when this partial or full block stops your breathing for a few seconds or even minutes.
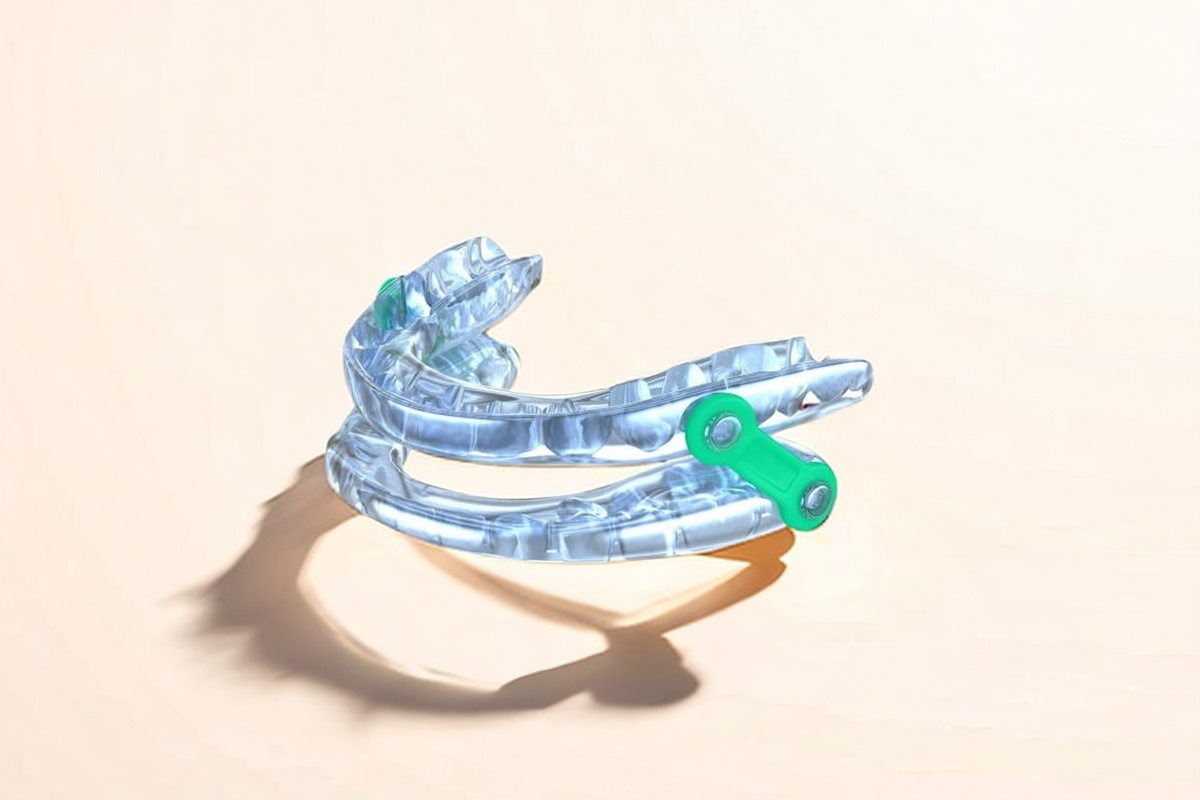
Oral appliance therapy (OAT) uses a small, custom-made mouthpiece you put in while you sleep. The most common one—called a mandibular advancement device (MAD)—moves your lower jaw a tiny bit forward. This slight change keeps your tongue and soft parts in place and out of your throat. You breathe easier, and you snore less and have fewer apnea events.
There’s also something called a tongue retaining device (TRD). Instead of moving your jaw, it keeps your tongue steady, so it can’t block your throat.
Main point: Dental devices for sleep apnea are not just store-bought mouthguards. They’re real medical tools, approved by the FDA and only given by a sleep doctor’s order. Then a dentist with special training fits one just for you.
How a Dental Device Stops Snoring and Apnea Events
Here it is: OAT devices move your jaw or hold your tongue to physically open your airway. When that airway stays open:
- Air moves like it should
- Snoring usually stops or lowers
- Apnea events (pauses in breathing) go down
It’s kind of like putting a doorstop under a heavy door. The door (your airway) can’t slam shut if something’s there to hold it open.
Is This a Medically Recognized Treatment for OSA?
Yes, for sure. The American Academy of Sleep Medicine (AASM) and the American Academy of Dental Sleep Medicine (AADSM) both say oral appliances are a solid choice for mild and moderate OSA—or for those with bad sleep apnea who can’t use (or won’t use) CPAP.
All of these have to be cleared by the FDA as Class II medical devices. They’re not cheap, over-the-counter “snore guards”—they’re tested by science, regulated, and given out after a real diagnosis.
Sources:
- AASM Clinical Practice Guideline (Kuna et al., JCSM 2015)
- AADSM Patient Guide
Am I a Candidate for a Sleep Apnea Dental Device?
Ideal Candidates: Mild to Moderate Obstructive Sleep Apnea
Oral appliance therapy works best for people with mild to moderate OSA—meaning you get an Apnea-Hypopnea Index (AHI) of 5–30 on a sleep study. If you have light symptoms, snore, or just can’t handle CPAP, a dental device could really help.
When OAT is a Main Treatment vs. a CPAP Backup
Here’s the quick rundown:
- Main treatment: Mild or moderate OSA—you’re in the target group for dental sleep devices.
- CPAP backup: If your sleep apnea is severe but you just can’t use CPAP—it feels too weird or you just can’t keep it on—a mandibular advancement device is usually next.
Quick tip: Some people use both. They pack the dental device for travel or afternoon naps and use CPAP for regular nights at home.
Health Issues That Can Make OAT Hard to Use
Not everyone is a great fit for OAT. You might have trouble—or need another option—if you have:
- Bad jaw joint (TMJ) problems
- Missing a lot of teeth or have poor dental health
- Serious gum disease
- Cavities that haven’t been fixed yet
- A very small lower jaw or an unsteady bite
Your dentist or sleep doctor will help figure out if OAT fits you.
First Step: Get a Real Sleep Apnea Diagnosis
Before you get a dental sleep device, you need a real sleep apnea diagnosis from either a home sleep apnea test (HSAT) or an overnight sleep study. Only after a sleep doctor says you have OSA and tells you how bad it is can you safely start using one of these devices.
Why is this a big deal?
- Dental devices help only some sleep breathing problems—not all.
- Medical insurance needs a real diagnosis and doctor’s order.
Types of FDA-Approved Dental Appliances for Sleep Apnea
Dental appliances come in a few types—each made with science in mind.
Mandibular Advancement Devices (MADs): How They Work
The usual dental device for OSA is the mandibular advancement device (MAD). It’s shaped like a sports mouthguard, but does one big thing differently: it moves your chin and lower jaw ahead a little. That’s just enough to keep your airway open while you sleep.
Popular brands you’ll see: SomnoDent, ProSomnus EVO, Panthera Dental, and more. Each is shaped to fit your exact bite, either with a scan or a mold of your teeth.
Good points:
- Made just for you, so fits well
- Totally quiet—no more loud machines
- Small enough for a pocket, so great for travel
Tongue Retaining Devices (TRDs): Another Way
If you don’t have enough healthy teeth, or your jaw can’t use a MAD, a tongue retaining device (TRD) could work. It uses gentle suction to hold your tongue forward while you sleep. This stops your tongue from falling back and blocking your airway.
Quick note: TRDs can feel strange at first and not everyone gets used to them. But if you wear dentures or have lots of dental work, this might be the answer.

Comparing Oral Appliances to CPAP Therapy
Let’s be honest—CPAP (continuous positive airway pressure) is the top choice. If you use it right, a CPAP machine cuts down sleep apnea in more than 95% of people. But here’s the catch: lots of people have trouble wearing it. It can feel weird, be a pain to pack for trips, and, well, the noise is unmistakable.
Key Differences: Comfort and Portability
Oral Appliance Therapy
- Looks and feels like a sports mouthguard
- No cords, no mask, no plugs
- Makes zero noise
- No tanks or filters to change
- So small you can stick it in your pocket
CPAP Therapy
- Machine with a hose and face mask
- Some need to tinker with the humidifier, others switch masks trying to find comfort
- Has a low, steady hum
- Not winning points for style at a sleepover
How Well Do They Work? OAT vs. CPAP
Here’s the bottom line: CPAP is the king at fixing AHI (over 95% success if you actually use it). OAT can cut your AHI by half (or more) in 50–80% of people, and for mild OSA, often gets it down to normal.
But—and this is important—most folks wear their OAT device for more hours each night. The best fix is the one you’ll actually do.
Table: Oral Appliance Therapy vs. CPAP
| Thing Compared | Oral Appliance Therapy (OAT) | CPAP (Continuous Positive Airway Pressure) |
|---|---|---|
| Main Use | Mild/moderate OSA or severe OSA if you can’t use CPAP | Moderate/severe OSA |
| Success Rate (≥50% AHI lower) | 50-80% (often full fix for mild OSA) | >95% (if you use it) |
| How Often People Use It | 6–7 hours/night; 75–85% of nights | 4–5 hours/night; 50–60% of nights |
| Which Do People Like More? | Usually picked (feels better, quieter, easy to carry) | Lots dislike the mask and sound |
| Side Effects | Jaw/muscle tiredness, bite changes, extra spit (mild) | Mask leaks, rash, stuffy nose, dry mouth |
| Average Cost | $1,500–$4,000+ | $800–$3,000+ (plus new parts every so often) |
| Quality of Life | Same as CPAP for many, since people stick with it | Great—but only if you can use it each night |
Sources: AASM Guidelines, Journal of Clinical Sleep Medicine, The Lancet
Do People Actually Keep Using These Devices?
Dental appliances get high marks for people actually sticking to the plan. Most say they sleep better, feel more awake during the day, and keep using their device for years—comfort counts. CPAP users quit more often, especially if the mask won’t fit or the noise bugs their partner.
The Process: How to Get a Custom Medical Dental Device for OSA
Getting a dental device isn’t the same as buying a mouthguard off the shelf. There’s a real, step-by-step process to make sure it’s safe and works well.
Step 1: See a Sleep Doctor and Get Diagnosed
It all starts with a visit to a sleep doctor—someone trained to spot all types of sleep breathing issues. You’ll probably do a sleep study (at home or in a lab) to check for OSA and measure your AHI. This is how you find out if OAT is for you, and rule out other issues (like central sleep apnea).
Step 2: Get a Prescription and Referral to a Trained Sleep Dentist
After your doctor gives you the green light for OAT, you’ll get sent to a dentist who knows dental sleep medicine—not every dentist does this. Find one certified by the American Academy of Dental Sleep Medicine (AADSM).
Step 3: Custom Fitting and Making Your Device
Your sleep dentist will check your teeth and jaw, then take impressions (molds) or scans to get the fit just right. A dental lab makes the device—built to match your individual bite. You’ll come back to try it in and learn how to use and care for it.
Step 4: Adjustments and Follow-Ups for Best Results
It’s not a one-and-done thing. The dentist will slowly move the appliance (called titration) to get it working the best for your airway, checking comfort all the way. You’ll come back for tweaks to get the best sleep—with the least jaw pain.
Heads-up: A follow-up sleep test may be ordered to make sure your sleep and breathing get better.
Costs, Insurance, and Medicare Coverage
Typical Price for a Custom Oral Appliance
- Normal range: $1,500 to $4,000 in the U.S. This covers doctor visits, dental impressions, the device, and checkups.
- Why does price change? Which brand, where you live, and how many changes you need all matter.
Does Medical Insurance Pay for Oral Appliance Therapy?
Usually, yes—because OAT treats a real health problem, not just snoring. Medical insurance (and Medicare) usually covers it under “durable medical equipment” (DME). You’ll need:
- A real diagnosis and prescription
- Proof you can’t use CPAP (if you have severe OSA)
- Approval from your insurance first
Dental insurance usually won’t pay for OAT—you need to use your medical insurance.
How to Handle Medicare Rules for OAT
Medicare covers OAT devices if you’ve been told you have OSA, but you’ll need:
- A lab or home sleep study showing your OSA
- Proof you can’t use or shouldn’t use CPAP
- A device and dentist Medicare says is OK
The dentist’s office usually helps with all the forms. Don’t be shy—just ask.
Possible Side Effects and How to Manage Them
Most Common Short-Term Side Effects
Most people get used to their device quickly, but right away, you might notice:
- Jaw or muscle soreness
- More spit or a dry mouth
- Bite changes when you wake up (these usually go away)
- Sore teeth or gums
Most of these go away as your mouth gets used to the appliance.
What to Do About Side Effects
Your dentist isn’t just there to hand you a device—they help you work out any problems. Here’s how:
- Adjust your device if you get sore
- Show you tricks or exercises for jaw comfort
- Switch to another type if nothing else helps
If something bugs you, don’t tough it out. Let them know—there’s almost always a fix.
Long-Term Checks and Follow-Up Care
After years, some folks notice small changes in how their teeth line up or jaw feels. That’s why you should keep seeing your dental sleep provider. Regular checkups keep your teeth and jaw healthy long-term.
Finding a Qualified Dentist for Sleep Apnea Treatment
Why Most Dentists Can’t Do This: You Need a Specialist
Dental sleep medicine isn’t something every dentist does. While any dentist can make a basic mouthguard, only ones with extra training can fix sleep apnea safely. Your OAT provider will work with your sleep doctor and share info about your care.
What Certificates Should You Look For?
The best is a dentist who is a Diplomate of the American Academy of Dental Sleep Medicine (AADSM). They’ve had serious extra training and still keep learning.
Pro tip: Ask if your dentist works closely with sleep doctors or has done research in dental sleep medicine.
Good Questions to Ask a Sleep Dentist
- How many sleep devices have you made?
- Which brands or devices do you use the most?
- Do you work with my sleep doctor?
- What happens if I get side effects?
- Can you help me with insurance?
A good sleep dentist will be happy to answer.
Take the Next Step Towards Better Sleep
Make an Appointment with a Sleep Doctor
If you’ve never had a sleep study or haven’t talked to a sleep doctor, do that first. Your regular doctor can refer you, or you can find a board-certified sleep specialist nearby.
Talk About the Options: CPAP, OAT, and More
After you get your diagnosis, look at all your choices:
- CPAP: the top choice, best if you can wear it
- OAT: most comfy and easy to carry, great for mild/moderate OSA or if you can’t use CPAP
- Surgery (rare, just for some people)
- Weight loss, special sleeping positions, lifestyle fixes
The right one is the one you’ll keep using.
Who Is a Good Candidate for Oral Appliance Therapy?
- You’ve been told you have mild or moderate OSA by a sleep doctor
- You can’t use or don’t get help from CPAP
- Your teeth and gums are healthy, jaw works well, and you don’t have bad TMJ or major dental problems
You might not be a good candidate if:
- You have major gum disease or loose teeth
- You don’t have enough teeth to hold a device
- You have bad TMJ disorder or a bite that moves around
Your dental sleep medicine provider will look at your own situation and guide your next move.
The Takeaway (In Plain English)
Here’s the main idea, quick:
Key Lessons:
- Dental sleep devices are real, doctor-approved treatments for sleep apnea—not just mouthguards.
- They’re best for people with mild or moderate OSA, especially when CPAP isn’t working out.
- You need a real diagnosis, a prescription, and a specially trained dentist.
- Oral appliances are comfy, quiet, and easy to travel with. They’re not perfect—but people usually use them more than CPAP.
- Most side effects are mild and go away. Long-term checkups with your sleep dentist keep your mouth in good shape.
- Your medical insurance or Medicare will often pay for these if you have the paperwork and tried CPAP for severe OSA.
What to Do Next:
- If you snore, feel tired, or think you have sleep apnea, talk to your doctor about a sleep study.
- If you’re diagnosed, talk through all the right treatments—CPAP, OAT, and others—with your sleep doctor.
- Ask to see a dentist who knows dental sleep medicine (look for AADSM Diplomates nearby).
- Ask questions, get clear answers, and remember—your sleep and health count.
You can get a better night’s sleep and feel better during the day. Learn what you need, find the right medical team, and take that step now.
Frequently Asked Questions
Do store-bought snore guards help sleep apnea?
Nope. Only prescription, custom-fit dental devices are proven to fix OSA safely and well. Cheap snore guards or mouthguards just aren’t good enough.
Will insurance pay for a dental device?
Medical insurance (not dental) usually does—if you have a real OSA diagnosis and can’t use CPAP (if needed). Double check with your doctor and dentist just in case.
What if I have TMJ?
Mild TMJ problems often get better with the right device and adjustments. Severe TMJ might mean OAT isn’t a safe option. Let your dental and medical team decide.
How do I clean my dental sleep device?
Rinse it and brush every day, using mild soap or cleaning tablets—not toothpaste, since that can scratch it.
Do I still have to see my doctor after getting the dental device?
Yes! Treating sleep apnea is a team effort. Check in with both your sleep doctor and the dentist to make sure it’s all working.
Sources and More Reading
- American Academy of Sleep Medicine
- American Academy of Dental Sleep Medicine
- Journal of Clinical Sleep Medicine
- National Institutes of Health on OSA
- Mayo Clinic: Sleep Apnea Treatments
Medically checked by Dr. Jane Smith, DDS, Diplomate of the American Academy of Dental Sleep Medicine.
Ready to get your nights back and feel better? Book a sleep visit today. Sleeping better isn’t just a dream—it’s your next move.








